(7 Min Read)
Are your systems addressing and supporting SDOH? Are you interested in bringing social determinants of health solutions to your member population?
Modern Americans are living longer, healthier lives than ever before because of social, public health, and medical technology advances. However, not every community has/will benefit equally from these improvements. Even when you account for economic status, there are still pervasive and well-documented health disparities that exist between racial and ethnic populations.
While 95 percent of U.S. health expenditures go toward medical care, most experts have long-agreed that medical services have a limited impact on health and well-being (HealthAffairs). What actually determines someone's health is a combination of genetic predisposition, behaviors, the medical services received, and the social and physical environment. These factors are collectively referred to as Social Determinants of Health (SDOH).
WHAT ARE SOCIAL DETERMINANTS OF HEALTH?
The World Health Organization (WHO) defines SDOH as "The conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels."
SDOH are the complex circumstances in which individuals are born and live that impact their health. They include intangible factors such as political, socioeconomic, and cultural constructs, as well as geographical conditions such as accessibility to healthcare and education systems, safe environmental conditions, well-designed neighborhoods, and availability of healthy food.
EXAMPLES OF SOCIAL DETERMINANTS OF HEALTH 
- Availability of Healthcare
- Availability of transportation
- Food insecurity and inaccessibility of nutritious food choices
- Governmental Policies
- Income level
- Educational opportunities
- Recreational and leisure opportunities
- Occupation, employment status, and workplace safety
- Gender inequity
- Racial segregation
- Access to housing and utility services
- Early childhood experiences and development
- Social support and community inclusivity
- Crime rates and exposure to violent behavior
- Neighborhood conditions and physical environment
- Access to safe drinking water, clean air, and toxin-free environments
SDOH AND VALUE BASED CARE
 Social determinants of health have proven to have measurable impacts on the health outcomes of patient populations. Currently, the healthcare industry is seeing a heightened focus on SDOH, including payer organizations, health systems, and independent medical groups.
Social determinants of health have proven to have measurable impacts on the health outcomes of patient populations. Currently, the healthcare industry is seeing a heightened focus on SDOH, including payer organizations, health systems, and independent medical groups.
As the healthcare industry shifts toward a greater focus on value-based care models, there is immense opportunity to integrate social determinants of health (SDoH) into future strategies. As value-based reimbursement increases, providers and health systems can better understand the attribution of issues that impact patients' & members' health, including their social barriers that could affect health outcomes.
America’s Health Insurance Plans (AHIP) has reported that many health plans are identifying at-risk populations, designing programs based on member needs, and mapping and cataloging existing community resources.Insurers have realized that by mitigating the negative impacts of SDOH significant benefits can be achieved that improve both access and outcomes for individuals while lowering overall costs.
Beginning in 2020, CMS plans to begin reimbursement for SDOH related benefits such as meals and transportation. Providing services to address the adverse social determinants of health will help organizations successfully participate in value-based pay arrangements and achieve the goals of the Quadruple Aim of better health, lower costs, and improved patient and staff experience.
Assessing Social Determinants of Health in Your Patient Population
FOCUS ON THE WHOLE PERSON
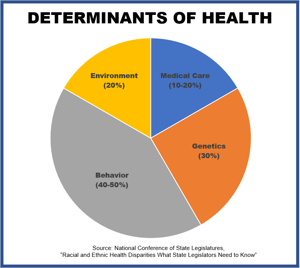 Medical care only accounts for 20% of health outcomes, so how do you address the remaining 80%?
Medical care only accounts for 20% of health outcomes, so how do you address the remaining 80%?
Healthcare organizations must now consider the whole person by utilizing a multidimensional approach and understanding the social issues that affect patients/members' health outcomes.
Studies have shown that behavioral and social determinants contribute to adverse health outcomes. These social determinants are barriers to positive outcomes and how you can systematically address real issues that could improve the health of your entire population.
A whole-person care approach that leverages SDOH data helps care teams identify non-medical issues that impact the patient, and work on those issues alongside medical care, ensuring the patient receives the most comprehensive care possible. Understanding how to leverage data from the various types of SDOH can help healthcare providers make informed decisions at the point of care to drive improved outcomes while lowering costs.
Being able to address real issues of determinants of health, providers, payers, and health systems will need to aim a whole-person care concept to address the challenge of obtaining positive health outcomes. Impresiv Health has those tools!
CAPTURING AND UTILIZING DATA
 Changes in the health care landscape are helping to generate greater interest in the collection and utilization of SDOH data to help improve the health of individuals and communities. However, efforts are continually thwarted by factors such as a lack of standardized terminology and tools.
Changes in the health care landscape are helping to generate greater interest in the collection and utilization of SDOH data to help improve the health of individuals and communities. However, efforts are continually thwarted by factors such as a lack of standardized terminology and tools.
In the past, social information captured in the medical records was limited to drug, alcohol and tobacco use, dietary and exercise habits, marital status, and occupation. Other nonclinical factors, such as economic stability, transportation access, food insecurity, or housing security, were rarely discussed or documented.
Now, with the push to improve outcomes by addressing these issues, organizations are facing barriers that range from data collection and aggregation to developing solutions that address these problems. Several national efforts now underway support standardizing SDOH data collection in electronic health records (EHRs) to make the data available to care teams.
One of the best places to start on your journey towards mitigating SDOH is in the collection of data. Ensure that steps are taken within your organization to collect and share quality data on all under-served populations. Accurate, consistent data provides a foundation from which effective programs and sound policy can be developed and implemented.
Once those details and data elements are known, health systems, providers, and technology must integrate and share information across those organizations. The data points need to be documented within a care plan that creates longitudinal records of combined social and clinical information.
Connecting social interventions to quality, satisfaction, and financial outcomes will improve and benefit health outcomes. SDOH-oriented technology should be designed to help providers and healthcare organizations manage problems related to health, not just disease states or conditions.
Electronic health record (EHR) systems such as Epic and Cerner offer software functionality that helps address SDoH with enhanced data collection, predictive insights, and other population health capabilities. Impresiv Health has helped organizations across the country develop, evaluate, and implement SDOH programs and the software that drives them.
TARGETED WORKFLOWS
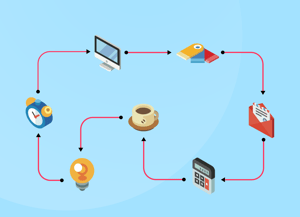 How do we bring together medical, behavioral, pharmacists, and community service providers across the continuum of care? We do it with comprehensive and targeted workflows. Organizations administering SDOH assessments often establish workflows to track patient needs and referrals, helping to standardize the process of screening patients and referring them to services, allowing the care team to better understand team members' roles and responsibilities.
How do we bring together medical, behavioral, pharmacists, and community service providers across the continuum of care? We do it with comprehensive and targeted workflows. Organizations administering SDOH assessments often establish workflows to track patient needs and referrals, helping to standardize the process of screening patients and referring them to services, allowing the care team to better understand team members' roles and responsibilities.
By implementing a screening process into your organization's workflow, you quickly gain a better understanding of what is important to the patient and identify social determinants that may be impacting their health status. A carefully designed care coordination workflow can allow the team to use data-driven work-lists that integrate tasks and actions for all the members of the core and extended care team.
SDOH factors can be combined with clinical risk factors to better identify and target the interventions needed for an individual. Stronger partnerships and ongoing communications between healthcare systems, social services, and community-based resources are vital. Understanding each organization's available resources, tracking what happens after each referral, and then folding that information back into the workflow is imperative to maintain continuity and to mitigate the gaps in the delivery of care.
TIPS FOR bUILDING A sUCCESSFUL sDOH STRATEGY
START SMALL
For organizations just beginning to leverage SDoH data, start small and strategically by capturing and addressing transportation and home support risks as part of inpatient discharge planning. Or, look to a known high-risk segment such as the diabetes population and begin examining underlying factors from medication adherence to housing that might be impacting that group.
EXPERT GUIDANCE
 Not sure where to start? Impresiv Health can help with that.
Not sure where to start? Impresiv Health can help with that.
Our consulting team of thought leaders and proven industry experts can work in tandem with your team to evaluate, craft, implement and launch your SDOH program utilize the ICoE. The Impresiv Center of Excellence (ICoE) is a comprehensive suite of proven solutions, best practices, tools, and resources designed to help your SDOH program become quickly operational, leading to better financial and population health outcomes.
Within the ICOE are research-driven workflows, scripting, questionnaires, protocols, and training resources that will quickly enable your internal teams to become self-sufficient and successful.
UTILIZE AVAILABLE RESOURCES
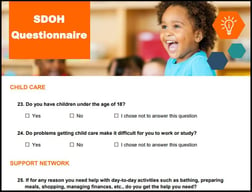 Impresiv Health's SDOH Questionnaire
Impresiv Health's SDOH Questionnaire
Impresiv Health's SDOH Questionnaire is designed as a starting point for the collection of SDOH data. It is composed of 43 questions that span 15 categories of need. Combine it with The Impresiv Center of Excellence (ICoE) for a complete profile of your members and their needs.
Download the SDOH Questionnaire
PRAPARE Implementation and Action Toolkit
 The Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences (PRAPARE) is a national effort to help health centers and other providers collect and apply the data they need to better understand their patients' social determinants of health, transform care to meet the needs of their patients, and ultimately improve health and reduce costs. PRAPARE is both a standardized patient risk assessment tool as well as a process and collection of resources to identify and act on the social determinants of health. The PRAPARE Implementation and Action Toolkit is designed to provide interested users with the resources, best practices, and lessons learned to guide implementation, data collection, and responses to social determinant needs.
The Protocol for Responding to and Assessing Patients' Assets, Risks, and Experiences (PRAPARE) is a national effort to help health centers and other providers collect and apply the data they need to better understand their patients' social determinants of health, transform care to meet the needs of their patients, and ultimately improve health and reduce costs. PRAPARE is both a standardized patient risk assessment tool as well as a process and collection of resources to identify and act on the social determinants of health. The PRAPARE Implementation and Action Toolkit is designed to provide interested users with the resources, best practices, and lessons learned to guide implementation, data collection, and responses to social determinant needs.
http://www.nachc.org/wp-content/uploads/2019/09/NACHC_PRAPARE_ALL.pdf
American Academy of Family Physicians (AAFP) — EveryONE Project Screening Tools
 The AAFP launched The EveryONE Project to help family physicians confront health disparities. The project focuses on providing family physicians and their practice teams with education and resources, advocating for health equity, promoting workforce diversity, and collaborating with other disciplines and organizations to advance health equity. The toolkit is designed to help family physicians address SDOH in their practices and communities.
The AAFP launched The EveryONE Project to help family physicians confront health disparities. The project focuses on providing family physicians and their practice teams with education and resources, advocating for health equity, promoting workforce diversity, and collaborating with other disciplines and organizations to advance health equity. The toolkit is designed to help family physicians address SDOH in their practices and communities.
https://www.aafp.org/patient-care/social-determinants-of-health/everyone-project/eop-tools.html
PROMOTE BUY-IN
Buy-in is the precious product of trust in a business relationship. Anyone who has implemented improvement programs understands that employees are the people who make changes happen. Getting positive employee engagement to support a change transformation is a common challenge faced by many organizations.
Most sustainable business transformations start at the top and trickle down. Meet with your leaders early on to explain key points of the proposed changes. Gaining support from leaders at different levels in the organization will make your plan stronger and ensure managers have time to prepare for questions that may arise throughout the process.
Click HERE to Read Impresiv Health's Blog: 8 TIPS FOR GAINING EMPLOYEE BUY-IN
ENCOURAGE COMMUNITY INVOLVEMENT
Breaking down silos between health and social service organizations, which typically have vastly different financing and IT systems, can be difficult. Work to develop partnerships with social services, community-based organizations, and government agencies. Begin by understanding the health needs of the communities you serve. Likely, you have already seen the impact of SDOH among your patients. In addition to listening to the perceptions of the communities served, there are multiple resources available in every community to learn more about the health of different groups.
LINK PATIENTS TO SDOH RESOURCES
Once you have identified patients who have screened positive for your selected SDOH need, the goal is to link the patient to appropriate resources. Providing the patient with a list of resources can be beneficial, but taking a more active role in arranging a resource alongside the patient and following-up to ensure benefits were accessed is likely to have a much more significant impact.
Many health care organizations lack a formal inventory of a community's available resources to address SDOH, as well as a standard process for tracking what happens after referrals. Often there is a lack of coordination between a community's social service organizations (such as food banks, homeless shelters, transportation agencies, etc.) and health care providers, many of which serve the same clients.
Building an adequate referral network of agencies that offer expertise, services, or resources that address identified social needs can be complicated and time-consuming. This network of services should be based on data reflecting the patient population's most urgent needs and cataloging the inventory of community resources. Health care organizations should dedicate resources to not only ensure that patients are referred to appropriate services but also to build inconsistent follow-up mechanisms to track connections to care and offer alternative options when necessary.
Learn More About Impresiv Health's Clinical Services
Never Miss Another Impresiv Health Blog
Sign up for our monthly newsletter to get the latest news, blogs, tips, and thought leadership from Impresiv Health.
References
AAF. (2020). Understanding the Social Determinants of Health - AAF. [online] Available at: https://www.americanactionforum.org/research/understanding-the-social-determinants-of-health/#_edn7 [Accessed 12 Feb. 2020].
Innovation.cms.gov. (2020). [online] Available at: https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf [Accessed 12 Feb. 2020].
Cms.gov. (2020). CMS finalizes Medicare Advantage and Part D payment and policy updates to maximize competition and coverage | CMS. [online] Available at: https://www.cms.gov/newsroom/press-releases/cms-finalizes-medicare-advantage-and-part-d-payment-and-policy-updates-maximize-competition-and [Accessed 12 Feb. 2020].
Healthaffairs.org. (2020). The Case For More Active Policy Attention To Health Promotion | Health Affairs. [online] Available at: https://www.healthaffairs.org/doi/10.1377/hlthaff.21.2.78 [Accessed 12 Feb. 2020].
Ncsl.org. (2018). Racial and Ethnic Health Disparities. [online] Available at: https://www.ncsl.org/portals/1/documents/health/HealthDisparities1213.pdf [Accessed 12 Feb. 2020].
The Henry J. Kaiser Family Foundation. (2020). Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. [online] Available at: https://www.kff.org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ [Accessed 12 Feb. 2020].
World Health Organization. (2020). About social determinants of health. [online] Available at: https://www.who.int/social_determinants/sdh_definition/en/ [Accessed 12 Feb. 2020].