We are in the midst of the Atlantic hurricane season, which runs June 1 to November 30, bringing with it the haunting reminder of how devastating a period of time this can be. Less than a year ago, hurricanes Harvey, Irma, and Maria tore across the US and its territories, accruing hundreds of billions of dollars in damages and lost productivity, displacing tens of thousands of people, and killing hundreds in the process. There are thousands of displaced families still in temporary housing to this day, many of whom unable to afford rent without federal assistance. For these families, accessing medical care is often an afterthought when so many other important aspects of their lives are uncertain and unstable.
The sobering fact is that socioeconomically disadvantaged families are more vulnerable during a catastrophic event. Research shows low income families, certain racial and ethnic groups, the elderly, children, people with disabilities, and those who live in poor quality housing and/or certain geographic locations are disproportionately affected by disasters in a variety of ways. For example, limited or no access to transportation—which is a negative factor in obtaining care before an emergency—is compounded during evacuation efforts in times of crisis. And for individuals with specialty needs, evacuation is more difficult.
As champions of their members’ quality of life, managed care organizations (MCOs) can revise their internal processes to account for the additional challenges these members face before, during, and after crises. Here are three steps you can take toward mitigating those challenges and better preparing your members and staff for what to do should a catastrophic event occur:
1. Configure your systems with a BI focus to identify your socioeconomically disadvantaged members. 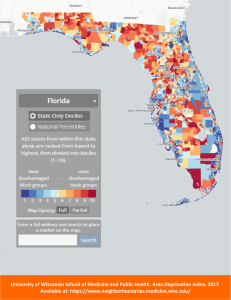
The healthcare ecosystem is trending toward providing more inclusive, equitable care to all member populations. But a caveat of the successful implementation of equitable practices is the collection of applicable data to facilitate seamless information and data sharing across the different departments in your organization. How can you structure a plan of care for members that meets their income level, educational background, language preferences, mobility, etc. if your systems aren’t configured to capture that level of data? Not only will this type of data help you provide the right care for your socioeconomically disadvantaged members; if configured correctly, it will also assist in designing specific adjustments that account for their needs during times of crisis.
For a starting point, you can use the Neighborhood Atlas—a National Institute of Health-funded tool that visualizes socioeconomic data—to search which areas within your coverage footprint are most disadvantaged based on socioeconomic measures. Then, use this information to find members who live in those areas and plan accordingly. Please note this is only a temporary solution, which does not internalize best practices for identifying specific members using specific data for specific outcomes. For a permanent, organization-wide solution, Impresiv Health can provide you with technical and advisory resources to help you update your systems, internal processes, and business intelligence practices.
2. Determine the incidence and method of delivery of care during and after a catastrophic event.
Adjust established plans of care based on the type of catastrophic event, the amount of damage expected, and the anticipated secondary hazards (like flooding and power outages after a hurricane) likely to occur. Each of these factors can affect how your members gain access to their medication, medical equipment, and care.
Your members’ acuity categories should give you insight into the level of adjustments that need to be made in the event of a disaster, with lower categories requiring fewer adjustments and higher categories requiring more. Once you’ve identified your socioeconomically disadvantaged members and the acuity category they belong to, craft a backup care plan that addresses their medical needs as well as their environmental and social needs.
For example, let’s say you have a low income, elderly member undergoing automated peritoneal dialysis at home with no access to personal transportation who typically has his monthly supply of equipment and fluids delivered to his residence. He belongs to a higher acuity category because of the need to perform dialysis daily and his lack of alternative resources. If a disaster stops traditional delivery services, how will he get his supplies? If required to pick up shipments at a distribution center, how will he get there? If the power goes out, what measures are in place to ensure his equipment can function? The answers to these questions and others will help you sort out the best route for alternate care during and after a crisis.
3. Communicate your disaster plans through the means that best suits the individual member.
You should review, test, and provide training on your disaster plans often, but don’t forget to include one of your key stakeholders: your members. According to a 2015 American Journal of Managed Care survey of AHIP members, “while 82% of plans participated in internal drills, fewer than 30% participated in drills with external stakeholders.” It is imperative that all members understand the various ways information will be communicated to them during and after an emergency, especially if telecommunications are down or not easily accessed, and how processes change during a particular crisis. But, you may have to adjust your communication methods to meet the needs of your socioeconomically disadvantaged members.
If members have language preferences other than English, for example, you should use patient navigators or translation services to communicate those plans. If a member does not have a phone, a representative may need to do a home visit to share updates. Using information on their preferences, you should revise your disaster plans to include the best means of communications for these members.
For more information…
At a high level, these general steps will help you address the needs of your socioeconomically disadvantaged members, but every MCO has its own unique member population and processes for serving that population. For more information on how to configure your systems, devise disaster and backup care plans, and/or source technical staff who fit your organization’s culture, contact us at info@impresivhealth.com.